What is melasma?
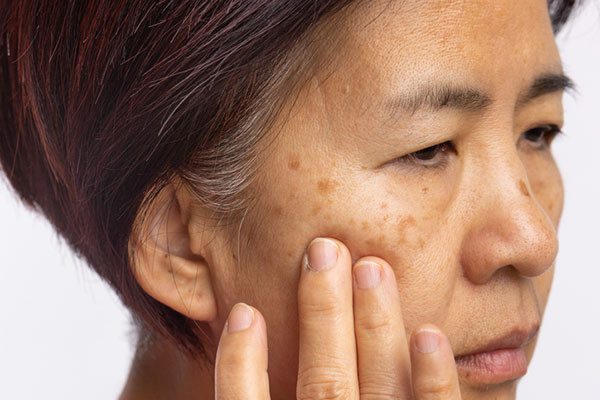
A condition in which brown patches appear on the face.
Melasma can be due to hormonal changes during pregnancy or from sun exposure. Women are much more likely than men to develop this condition.
Melasma is a common skin problem. The condition causes dark, discolored patches on your skin.
It’s also called chloasma, or the “mask of pregnancy,” when it occurs in pregnant women. The condition is much more common in women than men, though men can get it too.
Where does melasma most commonly occur?
Melasma appears most commonly on your cheeks, nose, chin, above the upper lip and the forehead. It sometimes affects your arms, neck and back. In fact, melasma can affect any part of your skin that is exposed to sunlight. That’s why most people with melasma notice that their symptoms worsen during the summer months.
How common is melasma?
Melasma is a very common skin disorder, especially among pregnant women. 15% to 50% of pregnant women get it. Between 1.5% and 33% of the population may get melasma and it happens more often during a woman’s reproductive years, and rarely happens during puberty. It usually starts between 20 and 40 years of age.
What are the types of melasma?
There are three types of melasma and they have to do with the depth of the pigment. A Wood lamp that emits black light may be used to determine the depth of the pigment. The three types are:
1. Epidermal: Epidermal melasma has a dark brown color, a well-defined border, appears obvious under black light, and sometimes responds well to treatment.
2. Dermal: Dermal melasma has a light brown or bluish color, a blurry border, appears no differently under black light, and doesn’t respond well to treatment.
3. Mixed melasma: Mixed melasma, which is the most common of the three, has both bluish and brown patches, shows a mixed pattern under black light, and shows some response to treatment.
What causes melasma?
There are two main causes of melasma: radiation, whether ultraviolet, visible light or infrared (heat) light; and hormones.
Ultraviolet and infrared radiation from the sun is key in making melasma worse. Other possible causes of melasma include:
• Antiseizure medications: Drugs that prevent you from having seizures may be a cause of melasma. An example of an antiseizure medication is Clobazam (Onfi®).
• Contraceptive therapy (birth control): Melasma has been observed in individuals who use oral contraceptive pills that contain estrogen and progesterone.
• Estrogen/Diethylstilbestrol: Diethylstilbestrol is a synthetic (man-made) form of the hormone estrogen. It’s often used in treatments for prostate cancer. Again, there’s a pattern between increased estrogen and melasma.
• Genetics: About 33% to 50% of people with melasma have reported that someone else in the family has it. The majority of identical twins both have melasma.
• Hypothyroidism: A condition where your thyroid is underactive.
• LED Screens: Melasma may be caused by the LED lights from your television, laptop, cell phone and tablet.
• Pregnancy: It is unclear why “the mask of pregnancy” happens to pregnant women. However, experts theorize that the increased levels of estrogen, progesterone and the melanocyte-stimulating hormones during the third trimester of pregnancy play a role.
• Hormones: Hormones like estrogen and progesterone may play a role in some people. Postmenopausal women are sometimes given progesterone, and have been observed developing melasma. If you aren’t pregnant, you likely have elevated levels of estrogen receptors found in your melasma lesions.
• Makeup (cosmetics): Some cosmetics can cause what’s called a phototoxic reaction.
• Phototoxic drugs (medicines that make you sensitive to sunlight): These include some antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, retinoids, hypoglycaemics, antipsychotics, targeted therapies and some other drugs.
• Skin care products: A product that irritates your skin in general will likely make your melasma worse.
• Soaps: Some scented soaps are thought to cause or worse melasma.
• Tanning beds: The UV light produced by tanning beds damages your skin just as bad as the UV light from the sun, and sometimes worse.
Is there a cure for melasma?
Treatments such as creams can help fade the discoloration, but treatments cannot make melasma go away forever. This skin condition can come back. It’s common for melasma to return when you spend time outdoors without protecting your skin from the sun.
In fact, many people who have melasma say the dark spots and patches become more noticeable during the summer and fade in winter. For this reason, it is important to use sunscreen every day and wear a wide-brimmed hat to keep the spots from getting darker or returning.
What questions might my healthcare provider ask to diagnose melasma?
• When did see the discoloration in your skin?
• Where are the discolorations located on your body?
• Is there a history of melasma in your family?
• Are you pregnant?
• What soaps do you use?
• What cosmetics/makeup do you use?
• Do you have any other skin disorders?
• Are you interested in prescriptions that may improve your melasma?
• Are you interested in procedures that may improve your melasma?
Can melasma go away on its own?
Yes, it’s possible that your melasma will go away on its own within a few months. However, it is not likely to go away while you’re pregnant or taking hormone contraceptives. Take preventative steps like avoiding sunlight to keep your melasma from getting worse or, if it does fade away, to keep it from coming back. Melasma can return.
Causes of Melasma
The pigmentation is a result of the overproduction of melanin. People who tan easily or have naturally brown skin are prone to melasma because they have more active melanocytes compared to people with lighter skin.
Melasma depends on your genetic predisposition. A few of the other triggering factors are:
Sun exposure:
Uncontrolled exposure to the sun is the leading trigger as UV light from the sun stimulates the melanocytes, increasing melanin production.
Hormonal changes:
Internal hormonal changes, as seen in pregnancy, stress, thyroid disorders as well as exogenous hormone treatments in the form of oral contraceptives, intrauterine devices, and hormone replacement therapy, are all implicated in the triggering of melasma.
Medications:
Certain medications like anti-seizure drugs and malignant drugs could also act as triggers.
Skincare products:
Scented soaps, toiletries, cosmetics, and skincare products that irritate the skin. This may increase melanin production and accelerate melasma symptoms.
Melasma in Men: Causes and Treatments
Melasma is a pigmentation disorder that occurs commonly in women. However, melasma in men is also common now. It is characterized by the appearance of dark patches on the skin, mostly on the face or areas exposed to the sun. Although harmless, melasma can lead to lowered self-confidence due to brown hyperpigmentation on the nose, forehead, or entire face. Here is an insight into the causes and treatments for melasma in men.
Causes of Melasma in Males
• Overexposure to the sun can lead to the appearance of dark spots or patches on the skin due to the generation of excess melanin. This hyperpigmentation is called melasma.
• Hormonal imbalance is another leading cause of melasma in men. Thyroid disorders can also cause melasma.
• Stress can lead to hyperpigmentation, leading to the appearance of dark patches on the skin. This is melasma.
• Some men are genetically more susceptible to hyperpigmentation. So, genetic susceptibility or family history is also a reason behind melasma.
• A less common but important cause of melasma in men is cosmetics. Certain cosmetics with harsh chemicals may lead to the appearance of dark patches on the face.
• Certain photosensitizing medicines can lead to melasma in men.
How is melasma treated? What medicines help?
The first thing you need to do to treat your melasma is to make sure that it doesn’t get any worse. Do this by avoiding the sun, tanning beds, LED screens, irritating soaps, and birth control that includes hormones. If you are exposed to the sun, be sure to wear sunscreen with iron oxides and an SPF of 30-50 applied every two hours, as well as a wide-brimmed hat. These steps may prevent your melasma from getting worse.
The second path to take is topical medications. Topical therapy using tyrosinase inhibitors prevents new pigment formations by stopping the formation of melanin (the dark color). Examples of tyrosinase inhibitors and other types of helpful agents include:
• Azelaic acid: This cream, lotion, or gel is applied twice a day. It’s safe for pregnant women to use.
• Cysteamine: A small study of 50 people found cysteamine cream to be more effective than a placebo.
• Hydrocortisone (a topical corticosteroid): Hydrocortisone helps fade the color caused by melasma. It can also lessen the likelihood of dermatitis that may be caused by other agents.• Hydroquinone: This medication is applied as a cream or lotion. It goes directly onto the melasma patches at night for two to four months.
• Methimazole: Methimazole is an antithyroid cream or an oral tablet. It’s known to help melasma that resists hydroquinone.
• Soybean extract: Soybean extract is thought to reduce the transfer of color from the melanocytes to the skin cells.
• Topical alpha hydroxy acid: Epidermal pigments can be peeled off. This cream or chemical peel removes surface skin.
• Tranexamic acid: This is a cream or injection, or oral medication.
• Tretinoin: This prescription is a topical retinoid. It’s effective, but can cause dermatitis and should not be used during pregnancy.
The combination of hydroquinone, tretinoin, and a moderate topical steroid has had the best effect on melasma.
Other agents that are being studied to improve melasma include:
• Absorbic acid (vitamin C).
• Arbutin.
• Deoxyarbutin.
• Glutathione.
• Kojic acid or kojic acid dipalmitate.
• Licorice extract.
• Mequinol.
• Resveratrol.
• Runicol.
• Zinc sulfate.
Are there any procedures that can help melasma?
Topical treatment isn’t your only option. There are some procedures that your dermatologist can do to improve your melasma.
• Chemical peel: In this procedure, your clinicians will put a chemical on your skin that may make it peel. The skin that regenerates should be smoother and more evenly colored.
• Light-based procedures like intense pulsed light, non-ablative fractionated lasers, and low fluence Q-switched lasers.
Maintenance therapy and prevention
After achieving improvement of melasma lesions, strict sun protection and maintenance therapy need to be continued. Skin lighteners other than hydroquinone can be used in combination with retinoids to maintain the results, and hydroquinone therapy may be used intermittently if needed.
What is the price of the treatment in India?
Treatment of melasma is a time taking process. The creams and steroids need to be applied for a minimum of eight to twelve months before they start to fade away. So, this incurs a cost for the multiple creams and doctor appointments. And, moreover, laser treatment of melasma is an expensive affair. There is a probable need for 3-4 treatments over 3-6 months for the patients. Roughly, the amount may reach up to Rs 50,000.
Are the results of the treatment permanent?
The outcome of the treatment is usually permanent if proper care and precautions are taken. Removal of pigmentation does not guarantee its longevity. The patches may again appear if the skin is exposed to severe sunlight or if there is some hormonal imbalance. To prevent such, the use of sunscreens and protective masks during long outdoor stays under the sunlight is essential.
Takeaway message about melasma
The key point in the management of melasma is to use sun protection all the time and to avoid other triggers such as hormonal medications when possible. Since none of the available treatments are a cure, prevention is the best option. People with melasma should see a board-certified doctor for evaluation and appropriate treatment regimens to manage melasma and maintain the treatment results.